As we age, our bones change. These changes can significantly impact our health and lifestyle. Seniors are especially prone to losing bone density. But what is bone density and why is it important?
Bones give our bodies structure and enable movement. Healthy bones can withstand normal stresses and resist breaking under pressure. By understanding bone health, you can lead a robust and independent life, with enhanced mobility and independence. As well as reduce the risk of fractures and bone health issues.
So let’s get into the role of bone density and how you can proactively maintain it in your senior years. It’s not just about living longer but living healthier and with a better quality of life.
Understanding Bone Density
You may see the terms “bone health” and “bone density” used interchangeably. But it’s worth noting they’re different concepts.
Bone health is a broader term encompassing various aspects of the overall condition and functionality of your bones. Including their strength, flexibility, and mineralization, as well as their internal structure and how quickly old bone tissue is replaced.
Meanwhile, bone density (or bone mineral density) is an aspect of bone health.
What is Bone Density?
Bone density refers to the amount of bone mineral present in your bone tissue. It’s a measure of how dense and strong your bones are. Imagine your bones as a honeycomb. Bone density assesses how closely packed the ‘honeycomb’ structures are. The denser these structures, the stronger and more resilient your bones are against fractures and breaks.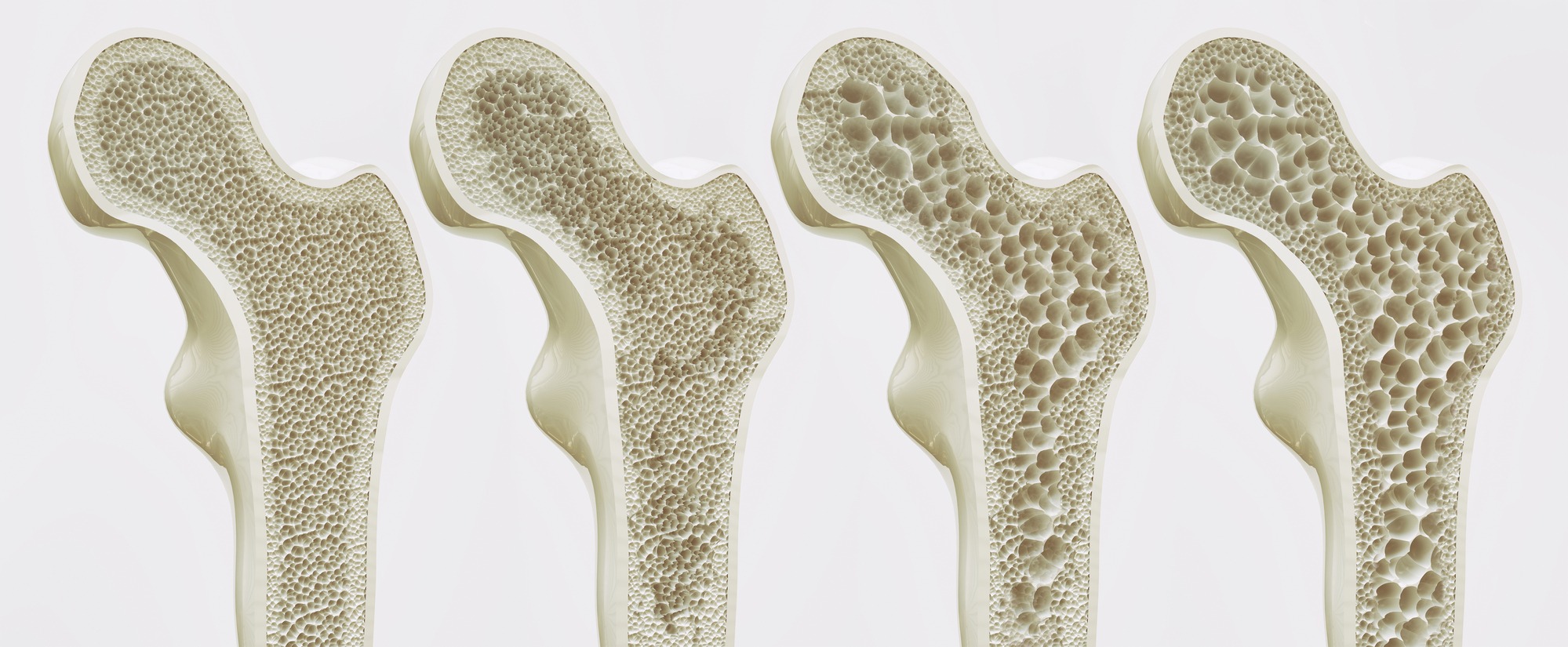
Bone density in older adults naturally begins to decrease as we age. Making them more susceptible to fractures and diseases like osteoporosis. However, the rate and extent of this decrease can vary significantly from person to person. Factors influencing this include genetics, diet, physical activity, and lifestyle choices.
Your bone density plays a pivotal role in healthy aging as it helps predict your risk of bone fractures. This is especially important for seniors. Where fractures have a more profound impact on your health and mobility.
Bone density helps you and your doctor make informed decisions about your bone health management. Whether you need to consider any lifestyle changes, preventive measures, or treatment plans if necessary.
Changes in Bone Density as We Age
The bone density in older adults undergoes a natural and inevitable transformation. Starting in our mid-30s, bone mass begins to decline gradually. For women, this process accelerates after menopause due to a decrease in estrogen, a hormone vital for bone health.
Then, as we continue to age, the balance between bone formation and bone resorption (the process by which bone is broken down) also shifts. Leading to an overall loss in bone density.
Why Bone Density Matters for Seniors
Lower bone density in older adults means your bones are more fragile and susceptible to fractures. Fractures, particularly in the hip and spine, can severely impact mobility and independence in seniors.
Link Between Bone Density and Osteoporosis
Osteoporosis is a medical condition characterized by deteriorated bone tissue and dangerously low bone mass. The word itself means “porous bones” and is directly linked to decreased bone density.
The condition occurs when the creation of new bone doesn’t keep up with the removal of old bone. Bones which lose their density (minerals and mass) become more porous, leading to decreased bone strength.
When that happens, the structural integrity of your bones is compromised. Putting you at risk of fracturing during minor falls or, in severe cases, simple actions like bending over or coughing.
Due to age-related loss of bone density in older adults, osteoporosis is very common among seniors. Particularly post-menopausal women. In Canada, it’s estimated that 1 in 3 women and 1 in 5 men contract osteoporosis.
Primary risk factors for osteoporosis:
- Age: The risk increases as you age.
- Gender: Women are more likely to develop osteoporosis, particularly after menopause.
- Family History: Genetics plays a role in the likelihood of developing osteoporosis.
- Body Frame Size: Individuals with smaller body frames tend to have a higher risk because they might have less bone mass to draw from as they age.
- Lifestyle Factors: Poor nutrition, physical inactivity, and smoking can increase the risk.
Fractures and Mobility
Unfortunately, osteoporosis usually doesn’t have any symptoms until the first fracture occurs. The most common fracture areas due to low bone density in older adults are the hip, wrist, and spine.

Sadly, osteoporosis leads to severe loss of quality of life and self-esteem. Seniors living with osteoporosis experience decreased mobility and physical changes. It also prevents seniors from being able to live independently.
Preventative Health Screenings for Bone Density
Because osteoporosis doesn’t have any symptoms, many don’t find out they have it until their first fracture. The only way to catch osteoporosis before it gets too severe is by measuring the bone density in older adults. This is done through specialized senior health screenings.
What Are Bone Density Tests?
Bone density tests, also known as bone mineral density (BMD) tests, are specialized procedures that measure bone density in older adults. These tests are crucial in diagnosing osteoporosis and assessing fracture risk.
Generally, women over 65 and men over 70 should consider getting a bone density test every couple of years. It may be recommended earlier for individuals with risk factors like a family history of osteoporosis.
The most common test is the Dual-Energy X-ray Absorptiometry (DEXA) scan. It uses low-dose X-rays to measure bone density, typically at the hip and spine. Your bone density is then analyzed based on a T-score, comparing your bone density to that of a healthy 30-year-old. Lower T-scores suggest weaker bones with a higher risk of fracture.
Osteoporosis Canada recommends getting a fracture risk assessment in conjunction with the results of BMD testing. The assessment evaluates whether certain factors will increase or decrease your risk of osteoporosis.
Maintaining and Improving Bone Density
Maintaining and even improving bone density in older adults is a proactive approach to ensure a healthier, more active lifestyle in senior years. It involves a combination of a balanced diet, proper exercise, and lifestyle choices that support bone strength.
Diet for Strong Bones
A diet lacking in essential nutrients can exacerbate the loss of bone density in older adults. While a balanced diet specific to seniors is necessary to stay healthy in general, certain nutrients are crucial for your bone health:
- Calcium: For building and maintaining strong bones
- Vitamin D: Helps the body absorb calcium
- Other Nutrients: Magnesium, Vitamin K, and proteins also play a role in bone health
Eat a diet rich in dairy, leafy greens, fish, and fortified foods that provide the calcium and other nutrients you’ll need. If you’re struggling to get enough from diet alone, use supplements for senior nutrition to help bridge the gap.
Exercise and Bone Health
Sedentary lifestyles contribute to faster bone density reduction. Weight-bearing exercises help maintain and even improve bone density. The best bone density exercises for seniors are ones that incorporate weights. Activities like walking, hiking, and low-impact aerobics are ok to start with. But lifting weights is the best way to strengthen bones.
Lifestyle Changes
Smoking and excessive alcohol consumption can negatively impact bone density in older adults.
Maintaining a healthy weight will also enhance your bone health. Being underweight can increase the risk of bone loss and fractures. Conversely, being overweight can put extra stress on the bones.
When to Seek Professional Help
Being aware of the signs of decreasing bone density in older adults and understanding when to consult healthcare providers can make a significant difference. Catching loss of bone density before it becomes a problem is important to be able to maintain a healthy and active lifestyle.
Signs of decreasing bone density:
- Frequent Fractures: Experiencing fractures from minor falls or injuries
- Height Loss: Losing height over time can be an indication of vertebral (spine) fractures
- Posture Changes: A stooped posture or noticeable curvature in the spine
- Back Pain: Chronic back pain, especially if it starts suddenly
Being vigilant about the signs of decreasing bone density in older adults and seeking timely professional advice are crucial steps in safeguarding your bone health.
If you’re a woman over 65 or a man over 70, you need to discuss a bone density screening with your doctor. Factors like a family history of osteoporosis, early menopause, or long-term use of certain medications (like corticosteroids) can also increase your risk.
Regular check-ups and conversations with healthcare providers help detect potential issues early. Identifying issues early will ensure appropriate measures are taken to maintain your bone strength and overall health.
Bone Density for Independent Living
It’s never too late to start focusing on your bone health. Whether you’re looking to prevent bone density loss or manage existing conditions. Every small step counts towards improving bone density in older adults. Ensuring your senior years are the best they can be.
At the Earl Haig Retirement Residence, we’re deeply committed to promoting the bone health of our residents. We understand that a wholesome diet is the foundation of good bone health. Our menus are thoughtfully crafted to support the well-being of our seniors.
Additionally, we champion senior fitness through a variety of group activities. One of our most popular is chair yoga. A gentle yet effective form of exercise that not only aids in maintaining bone density but also enhances flexibility and balance.
This combination of a nutritious diet and engaging physical activities creates an environment where our residents can thrive. Supporting their journey towards better bone health and an active, fulfilling lifestyle.
Remember to keep moving, eating well, and keeping up to date with your health check-ups.



